What is polycystic ovary & how common is it?
Polycystic ovary (PCO) also called Stein-Leventhal syndrome is a vast spectrum of disease affecting a women’s health ranging from:
- menstrual irregularities
- acne
- excess facial & body hair (hirsuitism)
- weight gain
- problems regarding fertility
It is found in 10-20% of women of childbearing age. Almost 75% of women with irregular menses and/or infertility may have polycystic ovaries, as determined with both radiological and biochemical criteria.
Women in their 20-30 seem to be more commonly affected, although it can affect any women of childbearing age group.
What exactly happens in PCO?
The exact cause for PCO is not known, although patients with PCO often have mother, sister or aunt with a similar problem. It is also more common in girls born of consanguineous parentage. To know this, we need to understand the normal ovarian anatomy.
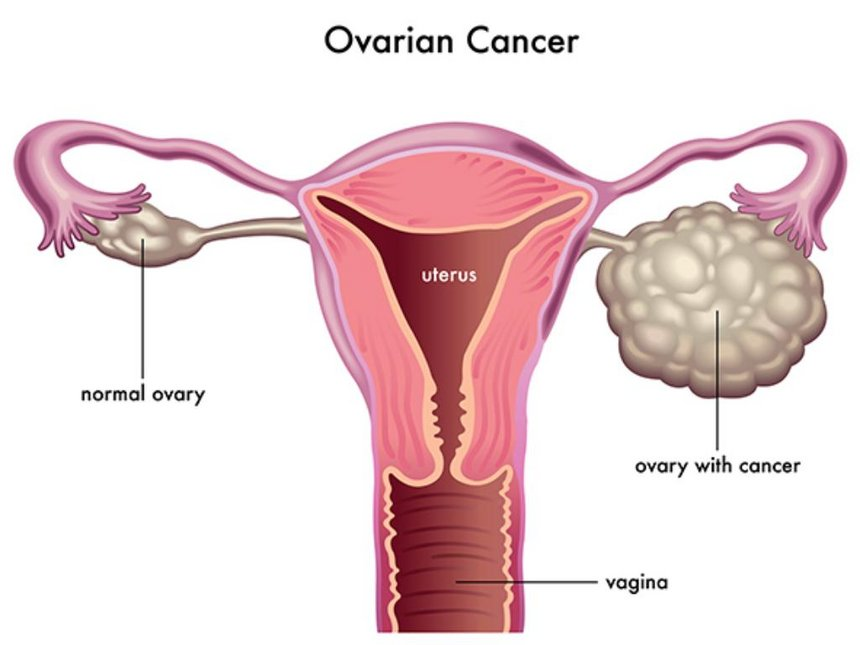
The ovaries are two small organs situated on either side of the uterus. The normal ovarian volume (length 3-5 cm, 1.5-3 cm in width, and 0.5-1.5 cm in thickness X 0.523) is around 10ml.
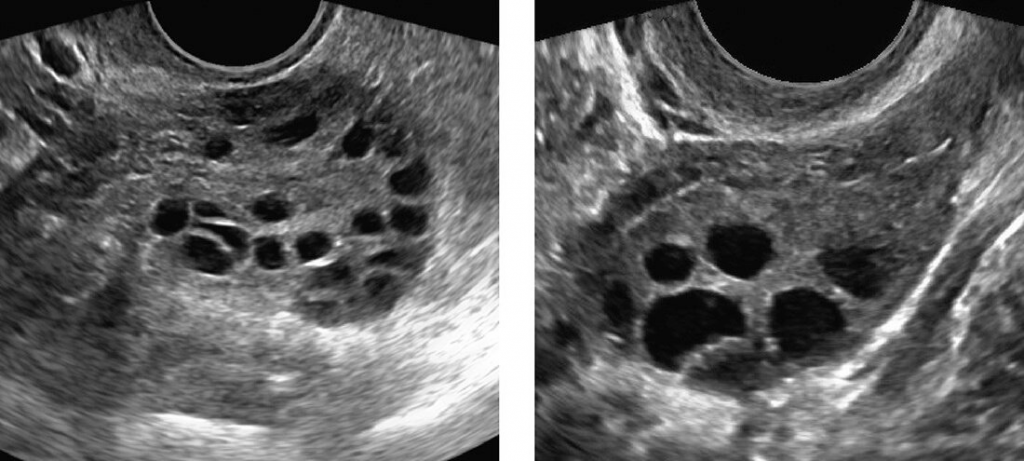
Ovaries have follicles, which are cysts filled with liquid that hold the eggs. Each month about 20 eggs start to mature, but usually only one becomes dominant. As one egg grows, the follicle accumulates fluid in it.
When that egg matures, the follicle breaks open to release the egg so it can travel through the fallopian tube for fertilization. When the single egg leaves the follicle, ovulation takes place.
In women with PCO, the ovary doesn’t make all of the hormones it needs for any of the eggs to fully mature. They may start to grow and accumulate fluid, but no follicle becomes fully mature.
Since no egg matures or is released, ovulation does not occur and the hormone progesterone is not made. Without progesterone, menstrual cycle is irregular or absent. Also, the cysts produce male hormones, which continue to prevent ovulation.
What are the common symptoms of PCOS?
These can be grouped into different categories:
- Menstrual irregularities – This is the most common feature where patients come in with irregular cycles/ scanty periods (70%).
- Features of androgen excess – 60% of women have hirsutism, 25% also suffer from acne/ male pattern baldness.
- Obesity & insulin resistance – 35% have features of obesity & insulin resistance. Clinical features of Insulin resistance is mainly limited to the black skin mark in the neck called Acanthosis Nigricans.
- Infertility due to anovulation is found in 30% of women.
What are the necessary investigations?
Laboratory investigations
Blood Tests
- Serum Testosterone concentration (May be normal or raised, levels may not reflect the degree of hirsutism)
- FSH/ LH
Pelvic ultrasound
- Ovarian volume (> 10cc)
- Presence of follicular cysts (>8 cysts)
Other investigations
- Blood glucose levels as upto 40% of women can have impaired glucose tolerance and 10% may have frank Diabetes mellitus
- Serum lipids
What are the treatment options available?
Most important treat of PCO is to understand the details and not to rely only on medications. First is a non-pharmacologic treatment like healthy lifestyle: Healthy eating, attempt to lose weight if you have extra, regular exercise, sleeping in time, etc.
Weight loss will reduce insulin resistance and thus hyperandrogenism. With a loss of 5% body weight, they show a 40% improvement in hirsutism.
Then comes pharmacological treatment, it depends on the problem you are facing, is it cycle, acne, excess hair or infertility.
1. Insulin Sensitizers
METFORMIN – Though this drug is mainly used in the treatment of Type 2 Diabetes Mellitus, it does not reduce the blood sugar in people with normal blood sugar levels.
It improves insulin sensitivity with a corresponding reduction in circulating androgens, decreases LH levels and increases Sex hormone binding globulin levels, thereby regulating menstruation improving ovulatory function and thereby inducing fertility.
It is usually started in 500mg/day and gradually increased to a maximum of 1.5 gm/day. A word of caution about the gastrointestinal side effects of metformin.
2. Hirsuitism
Drug treatment for hirsuitism should be combined with local measures. Drug treatment can alter only new hair growth and does not have an effect on established hair.
It takes 4-6 months for improvement to be visible and can recur once medications are stopped.
Adequate contraception is mandatory as the drugs used can be teratogenic. Local measures like hair removal depends on individual need.
3. Infertility
Weight reduction is a must as obesity adversely affects fertility outcome. Ovulation induction regimens are indicated with drugs like Clomiphene citrate or Gonadotrophin preparations. Laparoscopic ovarian diathermy is also used for restoring ovulation.
Studies have shown that Metformin should be continued until 12 weeks after conception in women with PCOS as it helps in continuing the pregnancy.
What is the prognosis for PCOS?
Cysts are benign and they do not cause many problems even if they stay back. Probably women with PCO are at increased for developing Type 2 Diabetes mellitus and Dyslipidemia in future. Hence they need to monitor for sugar and dyslipidemia.
Also see,